


- Stock: In Stock
- Model: 183562
0% Customers recommend this product
-
5 Awesome0%
-
4 Great0%
-
3 Average0%
-
2 Bad0%
-
1 Poor0%
Reviews Over Inflamin soup. rekt. 0.015 g No. 10
- (0)
Total Reviews (0)
click here write review to add review for this product.
Report this review.
Description
Translation of the instruction Mose
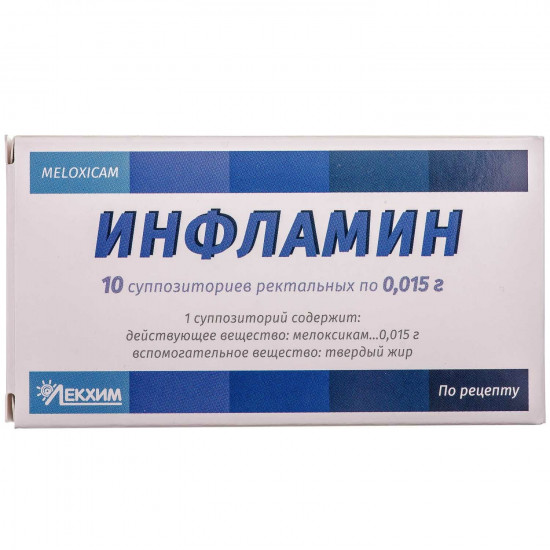
INFLAMIN suppositories rectal 0.015 gInstruction
On medical use of medicine
Inflamin
(inflamin)
Ingredients:
Active ingredient: meloxicam;
1 suppository supports a meloksikam of 15 mg;
excipient: solid fat.
Dosage form.
Suppositories rectal.
Main physical and chemical properties: suppositories of color, light yellow with greenish shade, puleobrazny form. Existence of a plaque on a suppository surface is allowed.
Pharmacotherapeutic group.
Nonsteroid anti-inflammatory and antirheumatic drugs.
ATH M01A C06 Code.
Pharmacological properties.
Pharmacodynamics.
Inflamin is the non-steroidal anti-inflammatory medicament of a class of enoliyevy acid having anti-inflammatory, analgeziruyushchy and febrifugal effect. Inflamin has high anti-inflammatory activity on all standard models of inflammation. The general mechanism of the specified effects can consist in Inflamin's ability to inhibit biosynthesis of prostaglandins — inflammation mediators.
Safe mechanism of action of Inflamin contacts selection inhibition of cyclooxygenase-2 (TsOG-2) in comparison with cyclooxygenase-1 (TsOG-1). The therapeutic effect of NPVS is connected with inhibition of synthesis of TsOG-2 whereas the inhibition of TsOG-1 results in side effects from a stomach and kidneys.
Selectivity of inhibition of TsOG-2 meloksikamy is confirmed toby many researchers both in vitro, and ex vivo. Inflamin (15 mg) mainly inhibits ex vivo TsOG-2 that is confirmed by big inhibition of products of PGE 2 in response to stimulation by lipopolysaccharide in comparison with products of thromboxane in the curtailed blood (TsOG-1). These effects are dose-dependent. Inflamin does not influence aggregation of thrombocytes or for a bleeding time at use of the recommended ex vivo doses whereas indometacin, diclofenac, an ibuprofen and Naproxenum considerably inhibit aggregation of thrombocytes and prolong bleeding.
Clinical trials established tolow frequency of gastrointestinal by-effects (perforation, formation of ulcers and bleeding) at use in the recommended doses of a meloksikam in comparison with standard doses of other NPVS.
Pharmacokinetics.
Meloksikam is well absorbed byfrom a digestive tract that is reflected in high absolute bioavailability (89%).
toshowed bioequivalence of suppositories to capsules. At use of one suppository the maximum concentration of a meloksikam in blood plasma is reached after 5–6 hours.
Stable concentration are reached byfor the 3-5th day.
Single dose of a daily dose causes concentration of medicament in blood plasma with rather small fluctuations between peak and its low point ranging from 0.8-2 mkg/ml for dosing on 15 mg (With min and the C max in stable equilibrium concentration).
Maximum stable equilibrium concentration in blood plasma after use of suppositories is reached byafter about 5 hours.
Continuous treatment during the long period (for example 6 months) did not leadto changes of pharmacokinetic parameters in comparison with parameters after 2 weeks of use of a meloksikam on 15 mg a day. Any changes are also improbable and lasting treatment more than 6 months.
Distribution. In plasma more than 99% contact proteins of blood plasma (mainly with albumine). Meloksikam gets into synovial fluid in concentration approximately twice smaller, than in blood plasma.
distribution Volume low, on average 11 liters. Individual deviations make 30–40%.
Biotransformation. Meloksikam is subject to extensive biotransformation in a liver. Meloksikam is almost completely metabolized to four pharmacological inert metabolites. The main metabolite, 5 -karboksimeloksikam (60% of a dose), is formed by oxidation of an intermediate metabolite 5 -hydroksimetilmeloksikam, is also allocated to a lesser extent (9% of a dose). The researches in vitro assume that CYP2C9 plays an important role in the course of metabolism whereas isoenzymes promote CYP3A4 to a lesser extent. The activity of peroxidase at patients, perhaps, is responsible for two other metabolites making 16% and 4% of the appointed dose respectively.
Removal. Excretion of a meloksikam — mainly in the form of metabolites — is carried out in identical quantity with urine and a stake. Less than 5% of a daily dose are allocated invariable in kcal whereas only traces of invariable components are allocated in urine. Elimination half-life makes about 20 hours.
Plasma clearance is 8 ml/min.
Special categories of patients.
Liver and renal failure. A liver or renal failure significantly do not influence pharmacokinetics of a meloksikam. In a terminal renal failure the increase of volume of distribution can lead to increase in concentration of a free meloksikam.
Patients of advanced age. The average plasma clearance in stable equilibrium concentration at people of advanced age was slightly lower, than at young people.
Clinical characteristics.
Indication.
Symptomatic treatment:
- a pain syndrome in osteoarthrites (arthroses, degenerative diseases of joints);
- pseudorheumatisms;
- ankilozivny spondylites.
Contraindication.
Known hypersensitivity to a meloksikam or to other components of drug.
Inflamin patients who have symptoms of bronchial asthma, nasal polyps, a Quincke's disease or a small tortoiseshell which are connected with use of acetylsalicylic acid or other NPVS as reactions of cross hypersensitivity are possible cannot appoint.
Also contraindications are:
- an active form or recent appearance of an ulcer in a digestive tract / perforation;
- an inflammatory disease of a large intestine in an active form (Crohn's disease or ulcer colitis);
- heavy liver failure;
- a heavy renal failure without dialysis use;
- manifest gastrointestinal bleeding, recent cerebrovascular bleeding or system disturbances of blood clotting;
- heavy uncontrollable heart failure;
- a proctitis in the anamnesis and rectal bleeding.
for use as anesthetic in the postoperative period at coronary shunting.
Interaction with other medicines and other types of interactions.
Other inhibitors of a prostaglandinsintetaza, including glucocorticoids and salicylates (acetylsalicylic acid): joint administration of inhibitors of a prostaglandinsintetaza because of synergy action can lead to increase in risk of bleeding and appearance of ulcers in a digestive tract therefore such combined treatment is not recommended. inflamin it is not recommended to apply together with other non-steroidal anti-inflammatory drugs.
Oral anticoagulants, antithrombocytic means, heparin for system use, thrombolytic means and also selection inhibitors of reversible serotonin reuptake: the risk of bleeding because of slowing down of function of thrombocytes increases. In need of such combined treatment it is recommended to carry out careful observation.
Lities: data on NPVS which increase the level of concentration of lithium in blood plasma take place. It is recommended to control lithium content in blood plasma in an initiation of treatment, at selection of a dose and at the treatment termination meloksikamom.
Methotrexate: NPVS can reduce canalicular secretion of a methotrexate, thereby increasing concentration it in plasma. For this reason it is not recommended to apply in passing NPVS to patients with a high dose of a methotrexate (more than 15 mg/week). The risk of interaction of NPVS and methotrexate should be considered also to patients with a low dose of a methotrexate, in particular to patients with impaired renal function. In case the combined treatment is required, it is necessary to control indicators of blood test and function of kidneys. It is necessary to observe cautions in case reception of NPVS and methotrexate lasts three days in a row as the plasma level of a methotrexate can raise and enhance toxicity. Though the methotrexate pharmacokinetics (15 mg/week) was not affected by the accompanying treatment meloksikamy, it is necessary to consider that the hematologic toxicity of a methotrexate can increase at treatment of NPVS.
Contraception: NPVS reduce efficiency of contraceptives.
Diuretics: treatment of NPVS of the dehydrated patients is connected with potential risk of appearance of an acute renal failure therefore before an initiation of treatment it is necessary to control function of kidneys, and further, at simultaneous use meloksikama and diuretics patients have to receive adequate amount of liquid.
Antihypertensive medicaments (for example beta blockers, APF inhibitors, vazodilatator, diuretics): NPVS reduce antihypertensive effect that is connected with the inhibiting influence on vazodilatatorny prostaglandins.
NPVS and antagonists of receptors of angiotensin-II and also APF inhibitors have synergetic effect on reduction of glomerular filtration. At patients with the existing renal failure it can lead to an acute renal failure.
Holestiramin connectsto meloksika in a gastrointestinal path, leading to its fast removal.
NPVS can increase nephrotoxicity of cyclosporine because of impact on renal prostaglandins that demands considerable control of function of kidneys at simultaneous use of drugs.
Meloksikam almost completely collapses by hepatic metabolism which about two thirds occur with mediation of P450 cytochrome (CYP) and one third — by peroksidazny oxidation.
Perhaps pharmacokinetic interaction of a meloksikam and other medicaments at a metabolism stage due to their influence on CYP 2C9 and/or CYP 3A4.
it is not revealedInteraction of a meloksikam with antacids, Cimetidinum, digoxin and furosemide at a concomitant use.
Cannot exclude interactions of medicament with oral anti-diabetic means.
Feature of use.
As well as about use of others npvs, at use of medicament it is necessary to watch closely a condition of patients with gastrointestinal diseases and those who accept anticoagulants. it is forbidden to appoint to meloksika if there are a round ulcer or gastrointestinal bleeding.
As well as at use of other NPVS, potentially lethal gastrointestinal bleeding, an ulcer or perforation can arise in the course of treatment at existence or without the previous symptoms or serious gastrointestinal diseases in the anamnesis at any time. The most serious consequences were observed at patients of advanced age.
byAt use of non-steroidal anti-inflammatory medicaments seldom or never observed serious skin reactions, some of them were lethal, including exfoliative dermatitis, Stephens-Johnson's syndrome and a toxic epidermal necrolysis. The highest risk of emergence of such reactions was observed in an initiation of treatment, at the same time in most cases such reactions appeared within the first month of treatment. At the first appearance of skin rashes, damages of mucous membranes or other signs of excessive sensitivity it is necessary to stop medicament use.
Non-steroidal anti-inflammatory medicaments can increase risk of emergence of the serious cardiovascular trombotichesky phenomena, a myocardial infarction and stroke which can be lethal. At increase in duration of treatment this risk can increase. Such risk can increase at patients with cardiovascular diseases or with risk factors of developing such diseases.
In view of possibility of side effects on skin and mucous membranes should pay special attention to emergence of such symptoms. At emergence of side effects the treatment meloksikamy should be stopped.
NPVS inhibit synthesis of renal prostaglandins which plays an important role in maintenance of a renal blood-groove. Patients with a reduced volume have blood and a reduced renal blood-groove use of NPVS can cause a renal failure which has reversible character after the termination of treatment of NPVS.
Greatest risk of such reaction takes place at patients of advanced age, at patients with dehydration, with stagnant heart failure, at patients with cirrhosis, with a nephrotic syndrome and chronic renal disturbances and also at the patients receiving the accompanying therapy with diuretics, APF inhibitors or blockers of receptors of angiotensin-II or after volume surgical interventions which led to a hypovolemia. Such patients need control of a diuresis and control of function of kidneys at the beginning of therapy.
In isolated cases of NPVS can be led to interstitial nephrites, a glomerulonephritis, renal medullary necroses or to development of nephrotic syndromes.
Dose of a meloksikam to patients with a terminal renal failure, being on dialysis, should not exceed 7.5 mg (in the form of tablets). For patients with insignificant or moderate renal disturbances the dose can be not reduced (level of clearance of creatinine more than 25 ml/min.).
byAs well as at treatment by the majority of NPVS, described isolated cases of increase in level of transaminases or other parameters of function of a liver. In most cases these deviations were insignificant and had temporality. At a resistant and considerable aberration of indicators of function of a liver the treatment meloksikamy should be stopped and carried out control tests. For patients with clinically stable course of cirrhosis it is not necessary to reduce doses of a meloksikam. The weakened patients need more careful observation. As well as at treatment by other NPVS, it is necessary to be careful concerning patients of advanced age at whom more probable depression of function of kidneys, a liver and heart takes place.
NPVS can strengthen a delay of sodium, potassium and liquid and to affect natriuretic effects of diuretics that can cause or strengthen warm disturbances or arterial hypertension. Carrying out clinical monitoring is recommended to such patients.
Inflamin, as well as any other NPVS, can mask symptoms of infectious diseases.
Use during pregnancy or feeding by a breast.
Inflamin is contraindicated toduring pregnancy.
Inhibition of synthesis of prostaglandins can have negative effect on pregnancy and/or development of an embryo and fruit. Data of epidemiological researches give the chance to assume about increase in risk of an abortion and development of heart diseases and gastrokhizis after use of inhibitors of synthesis of prostaglandins during the early period of pregnancy. It is considered that this risk increases with increase in a dose and duration of treatment.
B ІІІ a pregnancy trimester all inhibitors of synthesis of prostaglandins can create risk for a fruit:
- cardiopulmonary toxicity (with premature closing arterial channels and pulmonary hypertensia);
- disturbance of work of kidneys that can develop in a renal failure with oligogidroamniony.
Possible risks in deadlines for pregnancy for mother and the newborn:
- possible extension of a bleeding time, antiaggregation effect even at very low doses;
- oppression of reductions of a uterus that leads to a delay or delay in childbirth.
specific data on a meloksikama, NPVS is known that they can get into breast milk therefore to meloksika it is contraindicated to the women nursing.
Ability to influence speed of response at control of motor transport or other mechanisms.
is not presentData on influence of medicament on ability to drive the car or to work with other mechanisms. however at development of such by-effects as dysfunction of sight, dizziness, drowsiness or other disturbances from the central nervous system, is recommended to refrain from driving or work with mechanisms.
Route of administration and doses.
it is necessary forBefore use of a suppository:
- through perforation of the blister packing to tear off one suppository in primary packing;
- needs to be pulled further for edges of a film, breaking off it in different directions and to exempt a suppository from primary packing.
to adults and children from 12 years:
Osteoarthrites: 15 mg/days (1 suppository).
Pseudorheumatisms: 15 mg/days (1 suppository).
Ankilozivny spondylites: 15 mg/days (1 suppository).
Most recommended daily dose of a meloksikam for adults makes 15 mg.
As with increase in a dose and duration of treatment the risk of emergence of side reactions increases, it is necessary to apply the minimum effective daily dose during the short period of treatment.
At the combined purpose of various forms of medicaments of a meloksikam (capsules, tablets, suppositories, solution) the general daily dose should not exceed 15 mg.
Children.
to use Drug for treatment of children from 12 years.
Overdose.
toin case of overdose recommend the general supporting means as antidote is unknown. during clinical trials it was revealed what holestiramin accelerates removal of a meloksikam.
Side reactions.
from the system of blood and lymphatic system: deviations of indicators of blood test from norm (including a differential leukocytic formula), a leukopenia, thrombocytopenia, anemia.
Concomitant use of potentially myelotoxic drug, especially a methotrexate, can lead to emergence of a cytopenia.
from the immune system: anaphylactic reactions, anaphylactoid reactions and other allergic reactions of immediate type.
Mental disorders: confusion of consciousness, disorientation, change of mood.
Neurologic disorders: dizziness, drowsiness, headache.
from organs of sight: dysfunction of sight, the including illegibilities of sight, conjunctivitis.
from organs of hearing and a vestibular mechanism: vertigo, sonitus.
Cardial disturbances: heart consciousness.
Vascular disorders: increase in arterial blood pressure, inflows.
from the respiratory system, bodies of a thorax and mediastinum: bronchial asthma at patients with an allergy to acetylsalicylic acid and other NPVS.
from a digestive tract: gastrointestinal perforation, concealed or macroscopic gastrointestinal hemorrhage, duodenum ulcer, colitis, gastritis, esophagitis, stomatitis, abdominal pain, dyspepsia, diarrhea, nausea, vomiting, constipation, meteorism, eructation.
Gastrointestinal bleeding, an ulceration or perforation can be potentially lethal.
from a gepatobilliarny system: hepatitis, disturbances of biochemical indicators of function of a liver (for example increase in transaminases or bilirubin).
from skin and hypodermic cellulose: toxic epidermal necrosis, Stephens-Johnson's syndrome, Quincke's disease, bullous dermatitis, polymorphic erythema, rash, small tortoiseshell, photosensitization, itching.
from an urinary system: acute renal failure, changes of indicators of function of kidneys (increase in creatinine and/or urea of serum).
Use of non-steroidal anti-inflammatory medicaments can be followed by urination disorders, including a sharp ischuria.
General disturbances and disturbances in the injection site: hypostasis, burning, an itching in anorectal area.
Expiration date.
2 years.
Storage conditions.
to Storeout of children's reach at a temperature not above 25 °C.
Packing.
On 5 suppositories in the blister, on 2 blisters in a pack.
Category of release.
According to the prescription.
Producer.
Private joint-stock company lekkhim-Kharkiv.
Location of the producer and its address of the place of implementation of activity.
Ukraine, 61115, Kharkiv Region, city of Kharkiv, street Severina Pototskogo, house 36.
INFLAMIN solution for injections of 10 mg/mlInstruction
On medical use of medicine
Inflamin
(inflamin)
Ingredients:
Active ingredient:
1 ampoule (1.5 ml) of solution contains 15 mg of a meloksikam;
10 mg of a meloksikam contain1 ml of solution;
excipients: Megluminum, glikofurol, half-oxameasures 188, sodium chloride, glycine, sodium hydroxide, water for injections.
Dosage form.
Solution for injections.
Main physical and chemical properties: solution, transparent, yellow with a green shade.
Pharmacotherapeutic group.
Nonsteroid anti-inflammatory and antirheumatic drugs.
ATX M01A C06 Code.
Pharmacological properties.
Pharmacodynamics.
Inflamin is the non-steroidal anti-inflammatory medicament (NPVP) of a class of enoliyevy acid having anti-inflammatory, analgetic and antipyretic effects.
Inflamin showed high anti-inflammatory activity on all standard models of inflammation. As well as for other NPVP, its exact mechanism of action remains to unknown. However there is the general mechanism of action for all NPVP (including meloksika): oppression of biosynthesis of prostaglandins which are inflammation mediators.
Pharmacokinetics.
Absorption. Meloksikam is completely absorbed after an intramuscular injection. Relative bioavailability in comparison with that at oral administration — nearly 100%. Therefore to adjust a dose upon transition from use, intramuscular on the oral way, it is not required. After an intramuscular injection of 15 mg the maximum concentration in blood plasma makes about 1.6-1.8 mkg/ml and is reached in 1–6 hours.
Distribution. Meloksikam very strongly contacts proteins of blood plasma, mainly albumine (99%). Meloksikam gets into synovial fluid where its concentration in a half is less, than in blood plasma. Distribution volume low, on average 11 l after an intramuscular or intravenous way of use, also shows individual deviations within 7–20%. Distribution volume after use of repeated oral doses of a meloksikam (from 7.5 to 15 mg) is 16 l with deviation coefficient ranging from 11% up to 32%.
Biotransformation. Meloksikam is subject to extensive biotransformation in a liver.
byIn urine identified four various metabolites of a meloksikam which are pharmakodinamichesk inactive. The main metabolite, 5 -karboksimeloksikam (60% of a dose), is formed by oxidation of an intermediate metabolite
5 -hydroksimetilmeloksikama which is also allocated to a lesser extent (9% of a dose). The researches in vitro assume that CYP 2C9 plays an important role in the course of metabolism whereas CYP 3A4 isoenzymes play a smaller role. Activity of peroxidase at patients, perhaps, responsible for two other metabolites which make 16% and 4% of the appointed dose respectively.
Elimination. Removal of a meloksikam happens generally in the form of metabolites in equal parts to urine and a stake. Less than 5% of a daily dose are allocated in not changed view with a stake, the insignificant quantity is distinguished with urine. Elimination half-life makes from 13 to 25 hours depending on a route of administration (peroral, intramuscular or intravenous). The plasma clearance is about 7-12 ml/min. after a single oral dose, intravenous or rectal use.
Linearity of a dose. Meloksikam shows linear pharmacokinetics within a therapeutic dose from 7.5 mg to 15 mg after oral and intramuscular administration.
Special groups of patients.
Patients with a liver/renal failure. A liver and renal failure from easy to moderate degree significantly do not influence pharmacokinetics of a meloksikam. Patients with moderate degree of a renal failure had much higher general clearance. The lowered linking with proteins of blood plasma was observed at patients with a terminal renal failure. In a terminal renal failure the increase in volume of distribution can lead to increase in concentration of a free meloksikam. It is not necessary to exceed a daily dose of 7.5 mg (see the section "Route of Administration and Doses").
Patients of advanced age. At patients of male advanced age the average pharmacokinetic parameters are similar to that at male young volunteers. At patients of female advanced age the AUC value is higher and elimination half-life is longer in comparison with the corresponding indicators at young volunteers of both sexes. The average clearance of plasma in an equilibrium state at patients of advanced age was slightly lower, than at young volunteers.
Clinical characteristics.
Indication.
Short-term symptomatic treatment of a bad attack of a pseudorheumatism and ankylosing spondylitis when oral and rectal ways of use cannot be applied.
Contraindication.
- Iii a pregnancy trimester (see the section "use during pregnancy or feeding by a breast"); age of the patient up to 18 years; hypersensitivity to a meloksikam or other components of medicine, or to active agents with similar action, such, as npvp, aspirin. inflamin patients who had asthma symptoms, nasal polyps, a Quincke's disease or a small tortoiseshell after intake of aspirin or others npvp should not appoint; gastrointestinal bleeding or the perforation connected with the previous therapy npvp in the anamnesis; an active or recurrent round ulcer / bleeding in the anamnesis (two or more separate confirmed case of an ulcer or bleeding); heavy liver failure; a heavy renal failure, without dialysis use; gastrointestinal bleeding, cerebrovascular bleeding in the anamnesis or other disturbances of blood clotting; disorders of a hemostasis or simultaneous use of anticoagulants (contraindications are connected with way of use); heavy heart failure; treatment of perioperatsionny pain at coronary shunting (ksh).
Interaction with other medicines and other types of interactions.
Researches on interaction were conducted byonly with participation of adults.
Risks connected with a hyperpotassemia.
Some medicines or therapeutic groups can promote a hyperpotassemia: potassium salts, kaliysberegayushchy diuretics, inhibitors of angiotensin-converting enzyme (APF), antagonists of receptors of angiotensin II, non-steroidal anti-inflammatory medicaments (low-molecular or unfractionated) heparins, cyclosporine, takrolimus and Trimethoprimum.
Beginning of a hyperpotassemia can depend on whether there are related factors. The risk of emergence of a hyperpotassemia increases if to apply above-mentioned medicines concomitantly with meloksikamy.
Pharmakodinamichesky interactions.
Other non-steroidal anti-inflammatory medicaments (NPVP) and acetylsalicylic acid ≥ 3 g/days. The combination with other NPVP (see the section "Features of Use"), acetylsalicylic acid in doses ≥ 500 mg at one time or ≥ 3 g of the general daily dose is not recommended.
Corticosteroids (for example, glucocorticoids). Simultaneous use with corticosteroids demands care because of the increased risk of bleeding or appearance of ulcers in digestive tract.
Anticoagulants or heparin. Considerably the risk of bleedings owing to oppression of function of thrombocytes and injury of a gastroduodenal mucous membrane increases. NPVP can enhance effects of anticoagulants, such as warfarin (see the section "Features of Use"). Simultaneous use of NPVP and anticoagulants or heparin in geriatric practice or in therapeutic doses is not recommended. Due to the intramuscular introduction, solution for Inflamin's injections is contraindicated to patients that undergo treatment by anticoagulants (see sections of "Contraindication" and "Features of Use").
at use of heparin the care because of the increased risk of bleedings is necessary forIn other cases (for example, at preventive doses).
Thrombolytic and anti-aggregation medicines. The increased risk of bleedings by oppression of function of thrombocytes and injury of a gastroduodenal mucous membrane.
Selective Serotonin Reuptake Inhibitors (SSRI). The increased risk of gastrointestinal bleeding.
Diuretics, APF inhibitors and antagonists of angiotensin II. NPVP can reduce effect of diuretics and other antihypertensive medicines. At some patients with a renal failure (for example, at patients with dehydration or at patients of advanced age with a renal failure) simultaneous use of the APF inhibitors or antagonists of angiotensin II and medicines oppressing cyclooxygenase can lead to further deterioration in function of kidneys, including a possible acute renal failure which usually is reversible. Therefore the combination should be applied with care, especially to patients of advanced age. Patients need to receive adequate amount of liquid and also it is necessary to control function of kidneys after the beginning of joint therapy and periodically further (see the section "Features of Use").
Other antihypertensive medicines (for example, beta blockers). As well as at use of nizhezaznachenny medicines, decrease in antihypertensive effect of beta-blockers can develop (owing to oppression of prostaglandins with vasodilating effect).
Inhibitors of a kaltsinevrin (for example, cyclosporine, takrolimus). Nephrotoxicity of inhibitors of a kaltsinevrin can amplify NPVP by mediation of effects of renal prostaglandins. During treatment it is necessary to control function of kidneys. Careful control of function of kidneys, especially at patients of advanced age is recommended.
Deferasiroks.
Simultaneous use of a meloksikam and deferasiroks can increase risk of gastrointestinal side reactions. It is necessary to show care at combination of these medicines.
Pharmacokinetic interaction: influence of a meloksikam on pharmacokinetics of other medicines.
Lities. There are data on NPVP increasing the level of concentration of lithium in blood plasma (by decrease in renal excretion of lithium) which can reach toxic sizes. Simultaneous use of lithium and NPVP is not recommended (see the section "Features of Use"). If combination therapy is necessary, it is necessary to control carefully lithium content in blood plasma in an initiation of treatment, at selection of a dose and at the treatment termination meloksikamy.
Methotrexate. NPVP can reduce turbulyarny secretion of a methotrexate, thereby increasing concentration it in blood plasma. For this reason the accompanying use of NPVP is not recommended to patients who accept a high dose of a methotrexate (more than 15 mg/week) (see the section "Features of Use"). The risk of interaction of NPVP and methotrexate should be considered also to patients who at
Specifications
| Characteristics | |
| Active ingredients | Meloksikam |
| Amount of active ingredient | 15 mg |
| Applicant | Lekkhim |
| Code of automatic telephone exchange | M01AC06 Meloksikam |
| Interaction with food | It doesn't matter |
| Light sensitivity | Not sensitive |
| Market status | The branded generic |
| Origin | Chemical |
| Prescription status | According to the prescription |
| Primary packing | blister |
| Producer | AT LEKHIM-HARKOV |
| Quantity in packing | 10 suppositories (2 blisters on 5 pieces) |
| Release form | rectal suppositories |
| Route of administration | Rectal |
| Sign | Domestic |
| Storage temperature | from 5 °C to 25 °C |
| Trade name | Inflamin |












































